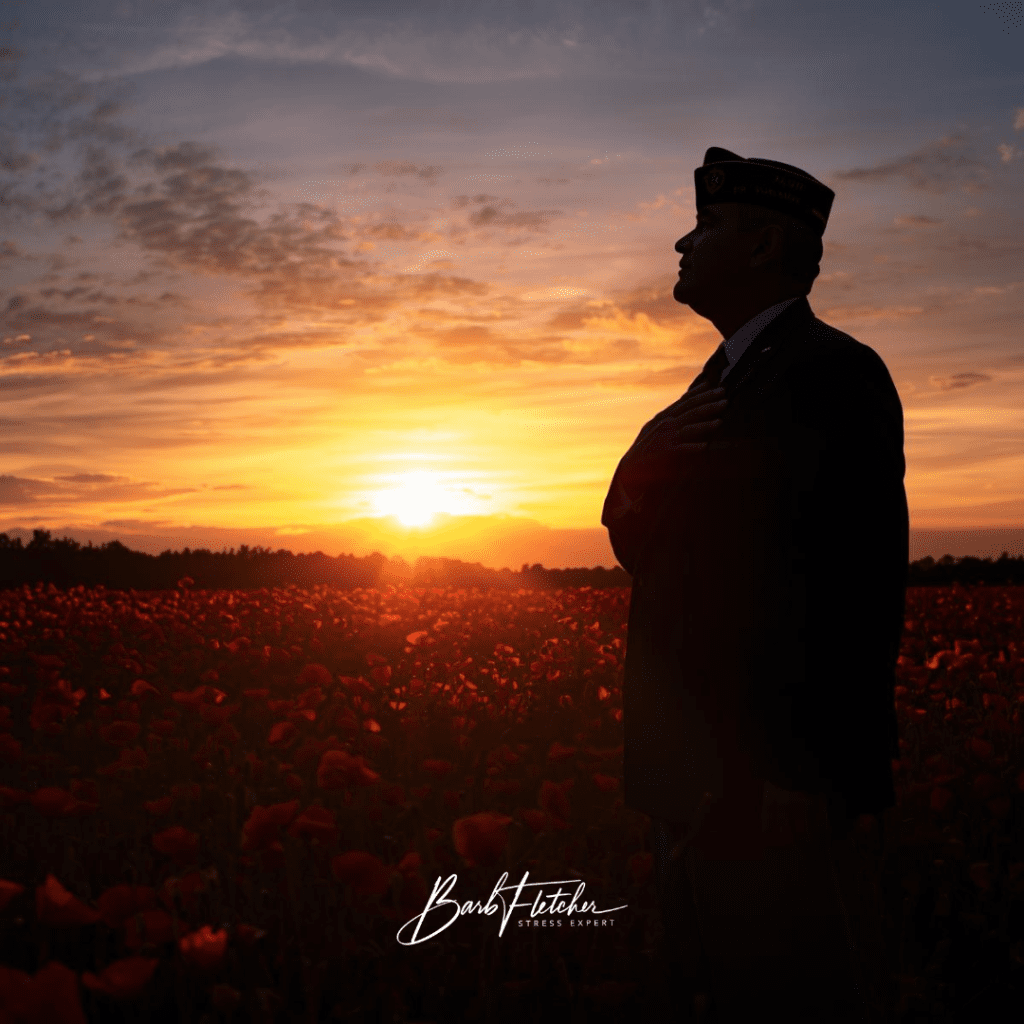
Some veterans tell me they can sense the mood of a room the moment they walk in. They know where the exits are, what sounds are off, and which conversations might turn. Even years after service, their system is still scanning.
I hear this often, and I want to name something clearly.
What you learned in uniform kept you alive. Hypervigilance was a skill. But your nervous system isn’t always told the mission has changed, and that can leave you on high alert long after the danger has passed.
Stress is a signal, not a weakness. And when the signal never shuts off, it takes a toll on your body, your relationships, and the way you connect with the people who love you.
Why Hypervigilance Persists Long After Service
The body does not differentiate between physical threat and emotional threat. This is one of the clearest lessons from trauma research. When the amygdala perceives anything unfamiliar or potentially unsafe, it signals the body to prepare for action. Heart rate rises, breath becomes shallow, muscles tense, and the vagus nerve drops out of its healthy rhythm.
When this happens occasionally, the system recovers. But when it happens repeatedly—day after day, deployment after deployment—it becomes familiar. Chronic alertness becomes the internal baseline.
Dr. Jorina Elbers explains that when the vagus nerve is repeatedly withdrawn, it becomes less available to keep the system healthy. Over time, the sympathetic system stays activated more than it should. Veterans often describe this as being “wired,” “on edge,” or “unable to shut it off.”
This is not a character flaw. It is physiology. And physiology can be retrained.
The Visible and Invisible Indicators of High Alert
Some signs are obvious. Others are subtle and easy to miss. Both matter.
Physical Indicators
Many veterans experience:
- Sleep disruption or light, restless sleep
- Elevated heart rate or a “fast idle.”
- Digestive issues, headaches, tension in the neck and shoulders
- Fatigue that doesn’t match activity levels
Low heart rate variability (HRV) is often part of the picture. HRV reflects the flexibility of your autonomic nervous system. Research shows that low HRV is associated with reduced resilience and difficulty regulating emotions. Veterans with a history of PTSD often show lower HRV, which aligns with the sensation of being on alert even at rest.
Emotional and Cognitive Indicators
Hypervigilance can show up as:
- Irritability or quick reactions
- Difficulty concentrating
- Feeling overwhelmed by noise or crowded spaces
- Trouble “coming down” after a stressful interaction
When your system is tuned for threat, the brain narrows attention. It becomes harder to access a broad perspective or intuition. As HeartMath describes, the cortex loses flexibility when stress floods the system.
Relational Indicators
This is where many veterans feel the deepest impact.
Trauma research shows how dysregulation affects connection. Social engagement requires a regulated nervous system; when we are in fight or flight, communication becomes harder. Small comments may feel like criticism, and closeness can feel like pressure.
Veterans often tell me:
- “I love my family, but sometimes they feel too close.”
- “I’m home, but I’m not really here.”
- “I react before I mean to.”
- This is not failure. This is physiology doing what it learned to do.

Statistics That Tell the Story
Several research trends highlight the hidden load many veterans carry:
-
HeartMath studies show a 45% improvement in sleep when individuals practice coherence tools regularly.
-
Veterans face higher rates of insomnia than the general population, often linked to chronic sympathetic activation.
-
HRV research shows that lower HRV predicts poorer resilience and greater emotional reactivity, conditions frequently observed in veterans with trauma histories.
-
Chronic autonomic activation increases cardiovascular risk. This is not just stress, but a measurable physical burden on the heart.
Your body carries the memories of service long after your uniform comes off, and your family often feels the secondary effects of that load.
How This Affects Families
Families sense emotional “weather” even when no words are spoken. When your inner weather is stormy, your partner or children may unconsciously adjust to avoid lightning. Over time, this becomes a pattern.
HeartMath describes this ripple effect beautifully: emotional states are contagious, and coherence strengthens communication and relationships.
Common family experiences include:
- Misreading tension as anger
- Walking on eggshells
- Feeling shut out
- Mistaking hypervigilance for disinterest or detachment
None of this means love is missing. It means your system is working overtime. And you can change that baseline.
Why Coherence Helps the Nervous System Settle
Coherence is not relaxation. It is a state of internal alignment where the heart rhythm becomes smooth and ordered. This pattern sends calming signals up through the vagus nerve to the brain, shifting the entire system toward balance.
Coherence is a superpower. It gives you access to your best thinking, steadiness, and the part of you that can respond rather than react.
Heart-Focused Breathing and Quick Coherence are bottom-up tools. They shift the body first, which then shifts the brain. As Dr. Rollin McCraty notes, changing the input from the heart and body can reset the inner baseline reference pattern that keeps the nervous system stuck in hypervigilance.
Even 60–90 seconds of coherence can:
- Reduce sympathetic activation
- Increase vagal tone
- Improve HRV
- Restore the capacity for connection
You do not need 30 minutes. You need moments. Moments change patterns.
A Simple Coherence Practice You Can Use Today
Here is a short practice I often teach veterans. It takes less than a minute.
- Shift attention to your heart area.
- Breathe a little slower and steadier. Imagine the breath moving in and out through your heart.
- Recall a renewing feeling. Something simple that evokes steadiness, appreciation, or ease. A place, a pet, a moment of quiet.
- Stay with it for 30 seconds. Let the body take the lead.
Notice what changes first. Breath. Muscle tone. Thinking. Any shift matters.
Life can be easier than we’ve been taught. Small practices nudge the system toward safety again.
An Invitation Forward
If you recognize yourself in these patterns, I want you to know something: there is nothing wrong with you. Your system is adapted to extraordinary circumstances, but you do not have to live in a permanent state of high alert.
Many veterans I work with have learned how to stand down internally, even when life around them is busy or uncertain. They learn to sleep more deeply, communicate more clearly, and reconnect with a steadiness they thought was gone.
If you would like support, I offer monthly coaching specifically for veterans. We focus on simple, practical skills grounded in HeartMath science—skills that help your nervous system remember it is allowed to rest.
You carried so much for so long. You deserve a space where your system can finally exhale.
If you are curious about building more steadiness, clearer thinking, and a deeper connection at home, I invite you to explore my veterans coaching program. It is a calm, confidential space to strengthen resilience, improve sleep, and retrain the nervous system through simple coherence practices.
Your service shaped you, but it does not have to define your baseline.
You deserve a life that feels lighter, clearer, and more your own.
If you are ready to take that step, reach out. I would be honored to walk with you.

Comment